Medicine Case Discussion
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent
Here we discuss our patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based input
This E log book also reflects my patient - centered online learning portfolio and your valuable inputs inthe comment box are welcome.
Name - S.Kavya, 8th sem
roll no - 121
I have been given this case to solve an attempt to understand the topic of "patient clinical analysis data " to develop my competency in reading and comprehending clinical data including clinical history,clinical findings, investigations and come up with a diagnosis and treatment plan
the topic of "patient clinical analysis data " to develop my competency in reading and comprehending clinical data including clinical history,clinical findings, investigations and come up with a diagnosis and treatment plan
LIVER ABSCESS
A 55 year old male patient who is a palm tree climber by Occupation
came on 17th April 2021 with the chief Complaints of
PAIN ABDOMEN SINCE ONE WEEK
DECREASE APPETITE SINCE ONE WEEK
FEVER SINCE 2 DAYS
HISTORY OF
PRESENTING ILLNESS
Patient was apparently asymptomatic 1 week back, then he developed pain abdomen in Right Upper Quadrant dragging type, non radiating, sudden onset, non progressive not associated with nausea / vomiting / loose stools
Fever since 2days which was high grade associated with chills and rigors not associated with cold , cough, SOB, Headache, neck pain, dizziness and sweating
No history of chest pain, palpitations,Burning micturition.
PAST HISTORY
Not a known Case of Diabetes, Hypertension, Tuberculosis, Epilepsy, CVDs
PERSONAL HISTORY
Diet - Mixed
Appetite - Decreased
Bowel and Bladder - Regular
Sleep - Adequate
Addictions - Chronic Alcoholic since 30 years. ( 1 bottle of Toddy per day), Consumes alcohol Occasionally
Beedis 10 per day since 30 years
FAMILY HISTORY
Not Significant
GENERAL EXAMINATION
Patient was Conscious, Coherent and Cooperative.
Well oriented to time, place ,person
Moderately built and moderately nourished
vitals
Temperature - 100 F
pulse - 76 bpm
Blood pressure - 90/ 70 mm Hg
Respiratory rate - 14 cycles per min
pallor - present
No signs of icterus, clubbing, lymphadenopathy, Edema
SYSTEMIC EXAMINATION
Abdominal Examination
Soft , Tender
Decreased movements in Right Upper Quadrant on respiration
No hernial orifices
Respiratory Examination
B/L reduced breath sounds on IAA (Rt more than left)
CVS Examination
S1 and S2 Heard
No murmurs
Liver abscess Aspirate
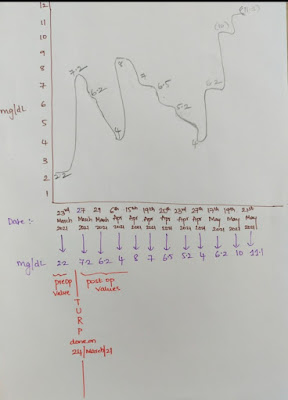
INVESTIGATIONS
During hospital stay
TREATMENT
Oral fluids - 2L
Injection pantop - 40 mg/IV/OD
Injection Ampicillin - 2G/IV/TID
Injection Clindamycin - 600mg / IV/TID
Tab Ultracet po/ sos
syrup Aristozyme 15ml po/TID
Protein powder 2 tbsp in one class of milk
Neb with budecort 12th hourly
Ascoryl 10ml po/TID
He was admitted in hospital for 10days and taken antibiotics treatment
when gastro opinion was taken pigtail catheterisation adviced ,but was not done as the abscess was not drainable
He was discharged on 26 April 2021 and from then he is on weekly follow up
Patient was discharged on 26 April 2021 with discharge medications and He was adviced for weekly follow up
Oral fluids
Protein powder 2tbsp in 1 glass of milk
Tab septran ds - ( 800mg/160mg) po/OD for 14 days
Tab Clindamycin - 600mg po/TID for 7 days
Tab Pantop 40mg PO/OD for 14 days
syrup Aristozyme - 10ml PO/TID for 7 days
Syrup Ascoryl - 10ml PO/TID for 5 days
Tablet zincovit - PO/OD for 15 days
Follow up on 3rd May 2021
Patient subjectively feeling better
No Complaints
O/E - pt was C/C/C
Temperature - Afebrile
Pulse - 78bpm
Blood pressure - 110/70 mmHg
- CVS Examination - S1 ,S2 Heard, No murmurs
- Respiratory Examination - BAE (bilateral air entry) + , NVBS
- Abdominal Examination - Soft and Non tender
- CNS Examination - NFND
Follow up on 12th May 2021
Patient subjectively feeling better
No Complaints
O/E - pt was C/C/C
Temperature - Afebrile
Pulse - 76bpm
Blood pressure - 100/70 mmHg
- CVS Examination - S1 ,S2 Heard, No murmurs
- Respiratory Examination - BAE +, NVBS
- Abdominal Examination - Soft and Non tender
- CNS Examination - NFND
Follow up on 19th May 2021
Patient subjectively feeling better
No Complaints
O/E - pt was C/C/C
Temperature - Afebrile
Pulse - 74bpm
Blood pressure - 110/70 mm
- CVS Examination - S1 ,S2 Heard, No murmurs
- Respiratory Examination - BAE +, NVBS
- Abdominal Examination - Soft and Non tender
- CNS Examination - NFND
Treatment
Tablet Metrogyl - 400mg PO/TID
Tablet pantop 40mg PO/OD
Tablet Ultracet 1/2 PO/QID
Injection Tremadol 1 amp in 100ml slow IV/SOS
plenty of oral fluids
USG guided Aspiration was done and pus sent for Culture and Sensitivity
Thank you for guiding me Dr.Vamshi sir






















Comments
Post a Comment