Medicine Case Discussion
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent
Here we discuss our patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based input
This E log book also reflects my patient - centered online learning portfolio and your valuable inputs inthe comment box are welcome.
Name - S.Kavya, 8th sem
roll no - 121
I have been given this case to solve an attempt to understand the topic of "patient clinical analysis data " to develop my competency in reading and comprehending clinical data including clinical history,clinical findings, investigations and come up with a diagnosis and treatment plan
the topic of "patient clinical analysis data " to develop my competency in reading and comprehending clinical data including clinical history,clinical findings, investigations and come up with a diagnosis and treatment plan
(Contains the information collated from Dr.Raveen sir PG1yr)
A 60 year old Female patient presented on 10th June 2021 with the chief complaints of -
Pain abdomen worsening since 1 week
Vomiting since 1 week - 5 to 10 episodes per day
Difficulty in passing urine since 4 days
History of presenting illness
Patient was apparently asymptomatic 1 year ago, then she developed mass per vagina which is progressively increasing in nature
She also gave history of decreased urine output since 3 months with complaints of hesitancy
No history of dribbling, urgency and frequency
There is a history of fever since 2months which is on and off with diurnal variation not associated with chills and rigors
also complaints of pain abdomen since 1 week which was gradual in onset and progressive , there are no aggravating or relieving factors and associated with vomiting 5 to 10 episodes per day since 1 week
there was associated generalised weakness and nausea
Past History
Not a known Case of Diabetes, Hypertension, Tuberculosis, Epilepsy, CVDs
No past surgical history and no history of blood transfusions
Personal History
Diet - vegetarian
Appetite - Normal
Bowel -Regular
Bladder - Hesitancy +
Sleep -adequate
No ill habits
Family History
Not significant
GENERAL EXAMINATION
Patient was Conscious, Coherent and Cooperative.
Well oriented to time, place ,person
Moderately built and moderately nourished
vitals
Temperature - 98.4 F
pulse - 98 bpm
Blood pressure - 120 / 70 mm Hg
Respiratory rate - 18cycles per min
pallor - present
No signs of icterus, clubbing, lymphadenopathy,
Edema - Bilateral pedal odema present since 2 months on and off on using medications
Systemic Examination
Abdominal Examination
Scaphoid abdomen, Tenderness in Hypogastric area
Bowel sounds heard
No Hernial orifices
Respiratory Examination
Bilateral air entry present and normal vesicular breath sounds
CVS Examination
S1 and S2 Heard
No murmurs
INVESTIGATIONS
Hemogram
Complete Urine examination
Blood Sugar
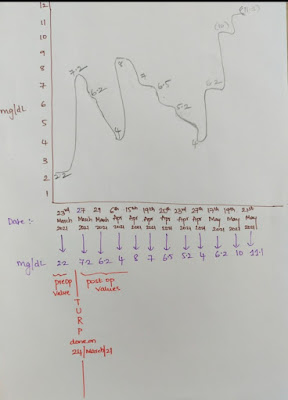
Blood urea
Serum creatinine on 10th june
Serum creatinine on 9th june
ABG
Liver function tests
Diagnosis
Post renal AKI secondary to severe bilateral Hydroureteronephrosis secondary to Uterine vagina prolapse
Treatment
20NS, 20RL - 75ml/hr
Injection pantop 40mg IV/ OD
Injection zofer 4mg Iv BD
Injection Tramadol 1 ampoule in 10ml NS IV BD
Tablet dolo 650 mg sos
Tablet Nitrofurantoin 100mg po BD
















Comments
Post a Comment