55 year old male presented with abdominal pain and dyspnea
A 55 yr old male patient who is labourer by occupation came with chief complaints of
abdominal pain since 3 days
Vomiting since 3 days
and shortness of breath since 1 day.
irritability since that morning
History of present illness
patient was apparently asymptomatic 1.5 year back. Then his family members noticed that he was becoming thin.So he was taken to general physician where he was diagnosed with diabetes mellitus for which he was started on oral hypoglycemic drugs.
3 months ago, he had fever for 3 weeks with cough associated with sputum, for which he consulted a doctor and was diagnosed with tuberculosis.He was started on anti tubercular drugs for a period of 6 months.
He is an binge drinker(once in 2-3 months).He was asked to quit drinking till the completion of ATT regimen.He stopped drinking alcohol for 2 months.
But on 1st January, he consumed alcohol continously for 2days without taking any food following which he developed abdominal pain which was insidious in onset,diffuse all over the abdomen. It was not associated with nausea and vomiting.
The followed day he developed a state of confusion and then next day he became breathless which was insidious in onset,persistent in nature and not relieved by any change in position.
He has history of weight loss.
Past history
Known case of DM since 1yr and taking oral hypoglycemics
Known case of TB and On ATT
Not a known case of asthma,epilepsy, CVD
Personal history
Diet - mixed
Appetite - normal
Bowel - regular
Bladder - increased frequency since 1 year
Sleep - adequate
Addictions - occasional binge drinker
No allergies
Family history
No History of DM,HTN, asthma, epilepsy, TB, CVDs
VITALS
Pulse rate:80 bpm
Respiratory rate:18 cpm
Blood pressure: 124/76 mm of Hg
Afebrile
No Pallor ,Icterus, Clubbing,Lymphadenopathy,Pedal edema, koilonychia
5:30-600
7:30- 390
8:30-380
9:30- 383
10:30- 382
11:30- 260
12:30- 210
1:30- 220
2:30- 206
3:30- 207
4:30- 147
5:30- 77
6:30- 121
7:30- 131
Systemic examination:-
CVS:
Precordium is normal
Thrills absent
Precordial heave absent.
S1 and S2 heard.
No murmurs heard.
Respiratory:
Chest is elliptical
Trachea: Central
Symmetrical expansion of chest.
Vesicular breath sounds heard.
No adventitious breath sounds heard.
No dull notes on percussion.
Abdomen examination:
Abdomen is scaphoid.
Moves symmetrically with respiration
Umbulicus is central and inverted
No scars or sinuses
No local rise in temperature
No tenderness
No organomegaly
CNS Examination:
Higher mental functions normal.
The patient is oriented to time, place and person.
When examined the patient was not irritable.
Meningeal signs were absent.
Cerebellar functions normal.
Cranial nerve examination normal.
Sensory examination: sence of fine touch, vibration, coarse touch are normal.
Motor examination:
Power: upper limbs: 5 bilaterally
Lower limbs: 5 bilaterally.
Tone: Normal
Reflexes: R. L
Biceps:. N. N
Triceps:. N. N
Knee. N. N
Ankle: N. N
Treatment:-
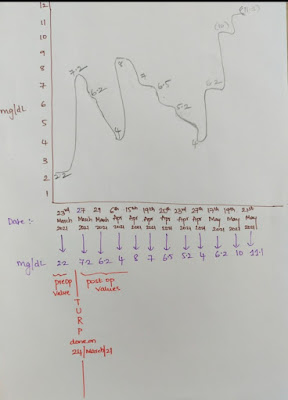
1. IVF- NS- 1L for 3hrs.
2. Inj HAI 6IU IV/STAT.
3. GRBS monitoring hrly.
4.IVF-5% Dextrose if GRBS<250mg/dl.
5.Inj THIAMINE 100mg in 100 ml NS/IV/BD.
6.Inj OPTINEURON 1 amp in 100ml NS/IV/OD.











Comments
Post a Comment